How long we live is not solely determined by what we do or who we are; it is determined by where we live. And where we live is often determined by who we are. Two ideas are central to understanding the connection between place, race, and health. First, unequal neighborhood conditions produce disparities in health outcomes. Bad neighborhoods are not the product of bad people, nor are some people intrinsically less healthy than others. Rather, some people live in places with health-supporting conditions like access to fresh food and taxation of tobacco products, and some do not. Second, differences across neighborhoods are not naturally occurring. They are the product of federal, state, and local policies interacting with the actions of private markets.
This policy brief reviews recent scholarship from members of the Diversity and Health Disparities cluster and offers important insights to meet the intertwined challenges of neighborhood inequalities and racial health disparities. The brief first reviews how the inclusion of place in research about health disparities initiates a new dialogue about the basis for persistent racial/ethnic health disparities that departs from discriminatory ideas linking them to what are thought to be natural differences. The brief next considers how residential segregation contributes to differences in neighborhood conditions and racial/ethnic health disparities. Taken together, the research presented in this brief provides new ways the think about health disparities and their causes, consequences, and potential remedies.
Introduction
A major misconception about health disparities is that they are a product of inherent differences between groups rather than a function of the unequal distribution of rights and privileges across populations. Poor health outcomes are a result of the myriad ways social and political systems are designed to marginalize certain groups by intersections of race, class, gender, or other social attributes. Neighborhoods manifest the differential outcomes of these systems in the quality of their streets and housing, exposure to toxic pollutants, and the presence of protective social networks among other social and physical characteristics, all of which impact health. Understanding how social and political systems perpetuate social inequality, and how social inequities determine disparities, will help inform effective structural solutions to close the gaps.
About the Haas Institute for a Fair and Inclusive Society
THE HAAS INSTITUTE for a Fair and Inclusive Society at UC Berkeley brings together researchers, community stakeholders, policymakers, and communicators to identify and challenge the barriers to an inclusive, just, and sustainable society and create transformative change. The Haas Institute advances research and policy related to marginalized people while essentially touching all who benefit from a truly diverse, fair, and inclusive society.
At the heart of the Haas Institute are seven clusters of teaching and research that focus on addressing society’s most pressing and pivotal issues related to vulnerable and marginalized populations. Together, the Haas Institute and the research clusters advance research and policy that address game-changing issues that are emerging
Haas Institute Diversity and Health Disparities faculty cluster
The findings in this report synthesize recent research from faculty working in the Haas Institute Diversity and Health Disparities research cluster, whose members are drawn from different disciplines across UC Berkeley. The Diversity and Health Disparities cluster addresses health inequities among racial/ ethnic minorities and other vulnerable populations through research, teaching, and policy activity on deeply rooted social inequalities within our society that result in disproportionate rates of illness and death in marginalized groups. These social inequalities include persistent poverty; unequal access to decent jobs, and quality education and housing; political disfranchisement; racial discrimination; and toxic living and working environments. The cluster focuses on two primary interest areas: (1) neighborhoods and the social economy of health disparities; and (2) health, human rights, and social inequality.
Why bring together neighborhoods, health disparities, and human rights?
A major misconception about health disparities is that health disparities are a product of inherent differences between groups rather than a function of the unequal distribution of rights and privileges across populations. Racial minorities aren’t likely to be sicker or have worse health outcomes because of biological differences. Rather, poor health outcomes are a result of the myriad ways social and political systems are designed to marginalize certain groups by intersections of race, class, gender or other social attributes. Neighborhoods manifest the differential outcomes of these systems in the quality of their streets and housing, exposure to toxic pollutants, and the presence of protective social networks among other social and physical characteristics, all of which impact health. Understanding: 1) how social and political systems perpetuate social inequality, and 2) how social inequalities and inequities determine disparities will help inform effective structural solutions to close the gaps.
How long we live is not solely determined by what we do or who we are; it is determined by where we live. And where we live is often determined by who we are.
Dr. Camara P. Jones, former president of the American Public Health Association, explains this phenomenon of structural inequality in her story, “A Gardener’s Tale”:1
A gardener has two flower boxes: one contains old, rocky soil and the other contains rich, fertile soil. The gardener has two packets of the same seeds in two colors, red and pink. Because the gardener prefers red over pink, the gardener plants the red seeds in the rich, fertile soil and plants the pink seeds in the old, rocky soil. The red flowers planted in the fertile soil flourish, while the pink flowers planted in the old soil are stunted and weak. Year after year, the same thing happens. Ten years later the gardener comes to survey her garden. Gazing at the two boxes, she says, “I was right to prefer red over pink! Look how vibrant and beautiful the red flowers look, and see how pitiful and scrawny the pink ones are.”
Jones’s allegory illustrates two ideas that are central to understanding the connection between place, race, and health.
First, unequal neighborhood conditions produce disparities in health outcomes. Bad neighborhoods are not the product of bad people, nor are some people intrinsically less healthy than others. Rather, some people live in places with health-supporting conditions like access to fresh food and taxation of tobacco products, and some do not. Manuel Pastor and UC Berkeley Professor and Diversity and Health Disparities cluster member Rachel Morello-Frosch argue, “These factors can be as critical to health outcomes as are access to medical insurance or health care, if not more so”.2 At a time when the United States spends 17.9 percent of the GDP on healthcare, it is critical for policymakers to shift the way policies are designed to reduce health disparities.3
Second, differences across neighborhoods are not naturally occurring. They are the product of federal, state, and local policies interacting with the actions of private markets. For example, the redlining maps created by the government-sponsored Home Owners’ Loan Corporation in the 1930s have had lasting effects on neighborhood disinvestment, residential segregation, and racial disparities in housing access and wealth accumulation4 —all of which affect health.5
Focusing research and policymaking on neighborhood conditions provides scholars, communities, and decision-makers the opportunity to understand and address the processes linking broader social and economic factors to health outcomes in very concrete ways.6
This policy brief reviews recent scholarship from members of the Diversity and Health Disparities cluster and offers important insights to meet the intertwined challenges of neighborhood inequalities and racial health disparities.
The brief first reviews how the inclusion of place in research about health disparities initiates a new dialogue about the basis for persistent racial/ethnic health disparities that departs from discriminatory ideas linking them to what are thought to be natural differences. Cluster members’ research findings show how neighborhood inequalities like safety and environmental exposures manifest in individual biology and physiology and how the distribution of diseases and poor health occur along lines that mirror other inequalities. This suggests that improving neighborhood conditions and building health equity can reduce disease and morbidity.
The brief next considers how residential segregation contributes to differences in neighborhood conditions and racial/ethnic health disparities. Greater segregation is connected to increased risk for extreme heat exposure, higher incidence of violence, and increased risk for hypertension. This research implies that housing policies and development decisions have a direct effect on health outcomes. Taken together, the research presented in this brief provides new ways the think about health disparities and their causes, consequences, and potential remedies.
What is a neighborhood?
Place and health literature relies on available data to analyze the relationship between the characteristics and features of a geographic area and health outcomes. These data are traditionally captured using geographic boundary indicators such as zip code and census tracts. Oftentimes, such measurements do not accurately reflect the lines that residents use to define their neighborhood or relevant policymaking boundaries such as congressional districts. This brief will use the term “neighborhood” to describe the organic area surrounding a particular place or group of people. The terms and definitions below represent the most frequently used measurements in place and health research to date.
Census tract
Region includes an average population of 4,000 residents. A “block-numbering area” is the equivalent in rural regions. Intended to demarcate relatively homogenous populations with regard to social and economic characteristics. Defined by the US Bureau of Census.A
Census block group
Region includes an average population of 1,000 residents. Block groups tend to be more homogenous, with regard to social and economic characteristics, than census tracts and can reveal hidden pockets of poverty and affluence. Defined by the US Bureau of Census.A
Census block
Region includes an average population of 85 residents. Block data are less useful for health research because relatively little data are reported at this level. Defined by the US Bureau of Census.A
Commuting zone
Region is a geographical aggregation of counties similar to metropolitan areas, but covers the entire United States including rural areas. The population of a commuting zone is not defined; it may range from 1,200 to more than 16 million residents.B
Zip code
Region includes a population of 30,000 or more residents. Zip codes are typically not homogenous in their sociodemographic characteristics. Defined by the United States Postal Service.A
Community-defined measure
Occasionally, research relies on study participants to define neighborhood boundaries. Participants in a 2012 study led by Nuru-Jeter and Richardson viewed the blocks on which they live as their neighborhood.C
Persistent Racial Health Disparities
PERSISTENT AND PERVASIVE racial/ethnic health disparities in the United States are a major public health concern. In 2012, the life expectancy of Black men was nearly 10 years shorter than the life expectancy of white women and infant mortality was twice as high for Black infants compared to white infants. Today, narratives about Shalon Irving, an epidemiologist at the Centers for Disease Control and Prevention with doctoral degrees in both sociology and gerontology who died from postpartum complications, and Serena Williams, the professional tennis player who experienced life-threatening blood clots the day after an emergency C-section delivery, illustrate the persistence of racial disparities in maternal mortality, postpartum complications, and medical care despite high educational achievement, physical strength, fame, and wealth.
Much of the existing health disparities research presents individual-level risk factors such as genetics, biology, income, and behaviors as explanations for differences in health outcomes.7 This research encourages leading health associations, like the American Heart Association, to recommend individual-level risk-assessment, such as instructing patients to use the online Heart Risk Calculator8 to predict their 10-year risk of heart disease or stroke, and individual behavior changes such as counting steps with a pedometer to decrease risk of obesity and heart disease.9
There is nothing incorrect about the American Heart Association’s recommendations, but they will only reduce poor health outcomes among individuals who have the resources, opportunities of choice, and the will to make the change.10 Improving health for people who lack such resources requires a different strategy and a different understanding of the underlying causes of risk and disease.
What makes these disparities especially troubling to policymakers, researchers, and public health officials, is their continued existence in the face of long-term national strategies to reduce them. Research cluster faculty Osagie K. Obasogie and Mahasin S. Mujahid, with Irene Headen from UC Berkeley School of Public Health, describe this paradox in a paper recently published in the Annual Review of Law and Social Science. Over the past 30 years, the US Department of Health and Human Service’s Office of Disease Prevention and Health Promotion has created 10-year strategic plans for improving population health and eliminating health disparities. A report summarizing progress towards the 2010 Healthy People goals shows improvements for many of the leading health indicators, but disparities between racial/ethnic groups and whites remain. American Indians, Alaska Natives, Hispanics, and Blacks had disparities amounting to 10 percent or greater for approximately 68 percent of the 111 Healthy People objectives assessed.11
Racial/ethnic health disparities also persist despite increasing investments in socioeconomic position. As explained by Health Disparities cluster member and UC Berkeley Epidemiology and Community Health Sciences Associate Professor Amani Nuru-Jeter, along with other researchers from UC Berkeley, Johns Hopkins University, and George Washington University in a recent Annual Review of Public Health publication, high socioeconomic position “does not buy the same level of health for African Americans relative to Whites”.12 In fact, research shows that significant racial health disparities exist at very high levels of income and education, which may be due to racism-related stress faced by people like Serena Williams and Shalon Irving who climb the social ladder. These differences can be difficult to see and are often underestimated, according to Nuru-Jeter et al.13
The cluster members’ observations point towards a need for new strategies to address the causes of racial/ethnic health disparities, which requires new research frameworks and methodologies.
Changing our understanding of chronic disease
RESEARCH LEADERSHIP by UC Berkeley Chancellor's Professor of Public Health and Diversity and Health Disparities faculty member Mahasin Mujahid has focused the attention of the American Heart Association on the influence of neighborhood conditions on cardiovascular health. In a 2017 scientific statement endorsed by the American College of Cardiology, Mujahid and a group of researchers representing the American Heart Association reviewed the state of cardiovascular health in African Americans. Findings show that African American men are more than twice as likely to die from coronary heart disease compared to white men1.1 and African American women are more than twice as likely to experience sudden cardiac death compared to white women.2.1 While these disparities can be partially explained by the higher prevalence of traditional cardiovascular risk factors among African Americans including hypertension, diabetes mellitus, and obesity, the researchers argue that disparities can also be explained by external sources of stress and adverse social determinants of risk.
Racial discrimination is a unique source of stress reported by African Americans and has been associated with hypertension, weight gain, adverse birth outcomes and persistent inflammation.3.1 African Americans are disproportionately exposed to adverse social determinants of health. Environments without health promoting resources is an important dimension of that risk. This includes places where access to supermarkets and healthier food options is limited,4.1 where advertising overwhelmingly promotes high-calorie low-nutrition foods and beverages,5.1 and where there is limited access to safe places for physical activity.6.1
Mujahid’s own research findings show the significant influence of neighborhood conditions on cardiovascular risk factors. Losing a neighborhood supermarket worsens the health of diabetic patients with poor baseline A1c measures;7.1 increasing individual and neighborhood-level safety over time is associated with decreasing BMI;8.1 higher neighborhood all-crime rates increase high stress among African American and Latina women;9.1 and neighborhood context may increase the risk of cardiovascular disease and contribute to racial/ethnic differences in health.10.1
If unfavorable neighborhood conditions increase the risk associated with poor cardiovascular health, then creating favorable conditions is a group- or place-level strategy for reducing cardiovascular disease. Furthermore, these advances will improve the context for biomedical interventions such as evidence-based therapies and clinic-based tools including screening and risk prediction,11.1 thus incentivizing healthcare providers and insurance companies to support neighborhood-level improvements in the name of health.
Neighborhood conditions: A common basis for multiple health disparities
RESEARCH SHOWS THAT neighborhood conditions and economic characteristics influence a variety of health outcomes and health behaviors. While the diversity of the causes and possible outcomes complicates research and study design, the close relationship between neighborhood conditions and health outcomes presents policymakers with a variety of ways to improve residents’ health.
Research findings of Diversity and Health Disparities cluster faculty Lonnie Snowden, UC Berkeley Public Health Professor, and Julian Chun-Chung Chow, Hutto-Patterson Charitable Foundation Professor at UC Berkeley School of Social Welfare, deepen our understanding of the complex relationship between neighborhood poverty, race/ethnicity, and mental health service use.12 Chow and Snowden compare the mental health service use of different racial/ethnic populations living in high- or low-poverty areas and find that disparities in emergency and inpatient service utilization and coercive referrals were more evident in low-poverty areas.
Their findings also reveal that racial/ethnic minorities who access mental health services are less likely than whites to have been referred by themselves, family members, or friends, as shown in Figure 2. Troublingly, Blacks and Hispanics are more likely than whites to be referred to mental health services by law enforcement. Snowden and Chow reason that the lack of tolerance for racial minorities in low-poverty areas makes these individuals stand out, which draws heightened attention from law enforcement, thus forcing racial/ ethnic minorities with mental illness into treatment services. These results imply the need to tailor mental health services to the unique needs of minority racial/ethnic groups in different settings, encourage appropriate pathways to mental health care in low-poverty areas, and prioritize programs in high-poverty areas that target racial/ethnic minority and immigrant children.
Neighborhood and social inequalities help explain high rates of asthma in racial/ethnic minority groups, as shown through research led by Jason Corburn, UC Berkeley Public Health and City & Regional Planning Professor and Haas Institute Diversity and Health Disparities research member. Corburn, Jeffrey Osleeb, and Michael Porter found that high rates of asthma hospitalization among New York City children can be predicted by having a low-income, being a minority, and living in substandard housing, as shown in Figure 3.13 Asthma rates in “hotspot” neighborhoods, where rates of asthma hospitalizations were statistically significant relative to the population, were nearly three times the national average, and hotspot residents were twice as likely to be African American and/or Latino.14
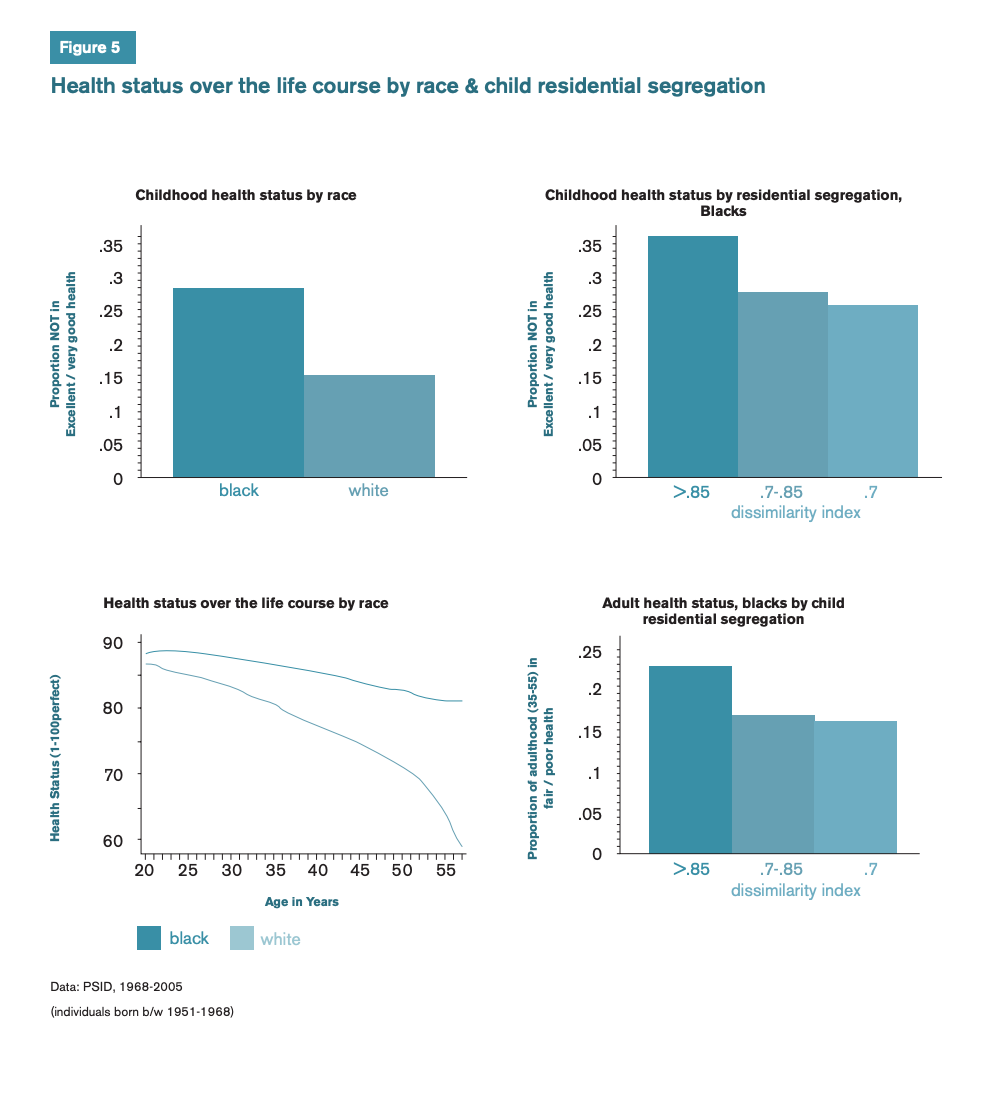
Research from UC Berkeley Public Policy Professor and Diversity and Health Disparities member Rucker Johnson describes a relationship between exposure to poor neighborhood conditions early in life and poor health later on. Johnson, Robert Schoeni, and Jeannette Rogowski followed the health trajectories of married couples and neighbors for 38 years and found that living in poor neighborhoods during young adulthood is strongly associated with negative health outcomes in later life.15 On average, the health status of Black people deteriorated 30 years faster than the health status of white people. This finding is consistent with the weathering hypothesis introduced by Arline T. Geronimus (1992), which posits that Blacks experience early health deterioration because of repeated exposure to social or economic adversity and political marginalization.16 Johnson’s findings build on his prior research that shows how neighborhood quality influences later-life health in ways that cannot be reduced to the characteristics of the individuals and families themselves, as illustrated in Figures 4 and 5.17
UC Berkeley Public Health Professor and Haas Institute Diversity and Health Disparities fauclty member Denise Herd, with Sylvia Guendelman, Paul Gruenewald, and Lillian Remer, produced research showing racial health disparities early in the life course. In a study examining the incidence of low birth weight among racial/ethnic groups living in the same area, Herd et al. found that rates of low birth weight among African Americans were lower if they lived in areas that were more densely populated, had greater income disparities, and had low rates of alcohol abuse or dependence.18 These relationships were different or absent for Hispanic and white women. The most surprising finding was that African American, but not white or Hispanic, women living in segregated areas had significantly lower rates of low birth weight infants. This finding builds on growing evidence of the benefits of high racial group density on African American health conditions.19 The results from Herd et al.’s study show us that the relationship between neighborhood conditions, race, and health outcomes is complex: conditions that may be beneficial for some groups are harmful or have no effect for others.
Research from the Haas Institute Diversity and Health Disparities research cluster demonstrates how the differences in racial/ethnic health outcomes are shaped by neighborhood-based factors such as concentration of poverty, population density, income disparities, and racial segregation. What’s interesting and complicated about these associations is that place and the people who compose a place are not mutually exclusive. Rather, they are part of a mutually reinforcing and reciprocal relationship.20 This is why reducing racial/ethnic health disparities will require cooperation and collaboration between many different stakeholders and decision-makers—city planners, physicians, lawmakers, community residents, and more.
Environmental inequalities contribute to unequal burdens of disease
RACIAL/ETHNIC health inequalities can also be explained by the spatial patterns of environmental inequalities. Disproportionate exposure to harmful environmental hazards, including air pollution, lack of green space, noise, and urban heat islands, occur in neighborhoods with high proportion of residents of color. The correlation between communities of color and high exposure to harmful environmental factors is what motivates Diversity and Health Disparities cluster member Rachel Morello-Frosch to investigate the causes and consequences of environmental disparities and identify opportunities for intervention and prevention at the community, regional, and state level.
Morello-Frosch regularly partners with community members through a research practice called community-based participatory research. Community members and university scholars form an equal partnership and rely on one another for skills, experience, and knowledge. Together, they identify a problem, gather data, analyze the data, share results, and use the findings to identify solutions. Made popular in academia by the work of UC Berkeley professor Meredith Minkler and Nina Wallerstein at the University of New Mexico,21 elements of a community-based approach can be found outside research in budget-making processes,22 youth-development,23 social movements,24 and public health departments.25
In 2006, Morello-Frosch partnered with residents living in Richmond, California who were concerned that their breast cancer diagnoses and problems with asthma, sore throats, rashes, and other cancers were related to their community’s close proximity to rail, truck, and marine shipping corridors, and the Chevron refinery in Richmond, one of the nation’s largest. Residents suspected that their proximity to pollution sources was related to the community’s demographics: 61 percent of residents identified as Latino, 18 percent as Black, and 3 percent as Asian American while 26 percent of residents had incomes below the federal poverty level ($17,603 for a family of four).26
Findings from the study revealed that communities neighboring polluting facilities experience higher exposure to a greater variety of pollutants than communities far from polluting facilities.27 Analysis of outdoor air quality detected 80 different compounds in Richmond compared to 60 in Bolinas, a predominantly white, rural community near the Pacific Ocean in Marin County. The research also showed greater concentration of compounds, particularly those associated with oil combustion activities, in Richmond than in Bolinas, as shown in Figure 6. The study found evidence of a strong difference between indoor and outdoor air quality measures. PM2.5 (particulate matter small enough to penetrate lung tissue) levels in nearly half of Richmond homes exceeded California’s annual ambient air quality standard as shown in Figure 6. This finding calls attention to the inadequacy of traditional environmental assessments, which use outdoor air quality to represent personal exposure, and calls for a change in institutional regulatory practices.
While this study did not provide evidence of a causal association between Richmond residents’ exposure to harmful compounds and health outcomes, it provided evidence of the impact that local sources of pollution have on nearby communities. Communities for a Better Environment, an environmental justice organization in Richmond, used these findings to advocate to the Richmond Planning Commission for restrictions on high-sulfur crude oil refining and to support their concerns about the effects of refinery emissions. Community participation throughout the research process gave community members the power to use research findings for health advocacy and measuring environmental exposures. This created an evidence base from which to draw hypotheses about disparities in racial/ethnic health outcomes.
Morello-Frosch has also found evidence linking noise pollution to racial/ethnic disparities. A growing body of research suggests that noise from transportation, industry, power generation, power tools and air conditioning generates biological stress and contributes to hearing loss and other health outcomes.28 Morello-Frosch wanted to know if noise exposure was divided along racial/ ethnic lines.
In 2017, Morello-Frosch and Joan Casey published findings from the first national study about noise pollution and racial/ethnic disparities. Their analysis of noise exposure by census block group indicated that neighborhoods with higher proportions of non-white and lower-socioeconomic status (SES) residents have higher levels of daytime and nighttime noise than neighborhoods with white and higher-SES residents.29 The most interesting finding from this study showed that block groups with the highest metropolitan area segregation had the highest estimated noise exposures—regardless of racial composition. In other words, while racial disparities in noise exposure exist regardless of a city’s segregation level, residents who live in more highly segregated cities experience greater noise exposure than those who live in cities with low segregation.
Just like their health-damaging counterparts, health-promoting environmental conditions are unequally distributed by neighborhood racial/ethnic demographics. In a recently published paper, Morello-Frosch highlights the inverse relationship between urban greenness and the percent of non-white residents over time. Between 2001 and 2011, non-white resident dominant neighborhoods lost more green space than white dominant neighborhoods, as shown in Figure 7.30 This finding implies that policies to increase greenness in disadvantaged communities are necessary, especially as climate change increases the frequency of extreme heat events.
When researchers and communities explore the relationship between environmental inequities, health disparities, and neighborhoods with high concentrations of people of color, they identify opportunities for coalition building between environmentalists, chronic disease advocates, city planners, housing developers, and public officials. This kind of broad coalition building is a bridging opportunity for groups with narrow interests to expand their goals and see the synergistic potential of coordinated policymaking.
Residential Segregation
Residential segregation is another lens through which researchers are exploring the relationship between disparities in neighborhood physical and social environments and disparities in health outcomes. This research often aligns with the interests of environmental justice, a concept and social movement focused on evidence showing that certain communities are subject to a disproportionate burden of pollution and contamination.31
Environmental Justice
Rachel Morello-Frosch’s explicit interest in advancing environmental justice is evident in research that shows how historical and contemporary racial inequality and discrimination shapes disparities in heat-related land cover.32 This 2013 study found that racial/ethnic minorities, particularly Hispanics and Asians, were more likely to live in areas with heat risk-related land cover, such as asphalt and concrete, than whites. While only 29 percent of whites lived in areas with no tree canopy and mostly covered with concrete or asphalt, 50 percent of Hispanics and 54 percent of Asians lived in areas with heat risk-related land cover.33 Figure 8 describes these data.
These findings have important implications for health. Extreme heat events are responsible for one in five natural hazard deaths in the United States.34 As climate change brings more extreme heat to cities, heat waves are expected to become more intense, more frequent, and longer lasting.35 Surfaces like asphalt and concrete contribute to high ground temperatures and tend to concentrate in areas called “urban heat islands” while trees lower surface and air temperature. In addition to Jesdale and Morello-Frosch’s findings, several other studies document racial/ethnic disparities in urban tree cover and find that racial/ethnic minorities are more likely to live in neighborhoods with lower tree coverage.36
In a paper focused on advancing theory and methods in residential segregation-based research, Rachel Morello-Frosch and Russ Lopez (2006) write, “examining [environmental justice] issues through the lens of racial residential segregation can offer new insights into the junctures of the political economy of social inequality with discrimination, environmental degradation, and health.” Indeed, research about residential segregation has led to findings that connect it to disparities in adverse birth outcomes, and increased risk of chronic disease, as well as increased risk of exposure to environmental hazards.37
Violent injury
Recent research from Haas Institute Diversity and Health Disparities research member and UC Berkeley Epidemiology and Community Health Sciences Associate Professor Amani Nuru-Jeter, along with Joshua Berezin, Sara Gale, Maureen Lahiff, Colette Auerswald, and Harrison Alter, finds that lower levels of neighborhood-level residential segregation are associated with lower levels of violent injury.38
Based in Oakland, the study used violent injury data from the detailed trauma registry at the Alameda County Medical Center’s Highland Campus to geo-code injury locations and link these locations to census block groups and determine the number of violent injuries per block group. The research team calculated residential segregation using a diversity composite measure that ranges from zero to one, with one representing maximum diversity (all groups are represented in equal proportions in the geographic area).39 Figure 9 presents these data.
Results from this study are consistent with a large body of research showing that lower levels of segregation (or higher levels of diversity, as presented in this study) are associated with lower levels of violence, particularly for predominantly Black and predominantly Hispanic neighborhoods. This finding challenges the idea that high neighborhood diversity is a destabilizing force and suggests that it may actually be protective.
Scholars debate the effects of neighborhood diversity on trust. Some, like Robert Putnam, argue that increased diversity leads people to “hunker down” and withdraw from the community—which means that Nuru-Jeter’s results could be interpreted as evidence that lower rates of violence in highly diverse neighborhoods are the result of decreased social interactions. Other experts argue that increased diversity fosters neighborhood trust and is a driver behind lower rates of violence in those neighborhoods. Nuru-Jeter’s research implies that decreasing segregation, or increasing resident diversity, creates positive neighborhood conditions like lower rates of violence, which are good for all residents’ health.
Income Inequality & Mortality
Residential segregation is not only racial, it is also economic. William J. Wilson’s seminal work The Truly Disadvantaged presents evidence of the way inner-city communities became more economically segregated as a result of the decline in low-skilled manufacturing jobs, which contributed to high rates of unemployment and white-flight.40 As economic segregation increased, so did income inequality.
Income inequality is a significant predictor of population health: greater income inequality is associated with poorer population health status.41 But the effects of income inequality cannot be separated from the role of race and ethnicity, two long-established correlates of mortality.42 Amani Nuru-Jeter, Chyvette Williams, and Thomas LaViest combined Wilson’s perspective with Massey and Denton’s argument that residential segregation is fundamentally racial to explain why the association between mortality and income inequality is different for Blacks and whites.43
In a national, cross-sectional ecological study, Nuru-Jeter et al. examined the association between income inequality and mortality among Blacks and whites separately.44 Their data showed that racial segregation explained the income inequality and mortality association for Blacks but not for whites, suggesting that racial segregation is potentially more harmful for Blacks than income inequality. Furthermore, the study showed that the association between income inequality and mortality was protective for whites, meaning white mortality rates decrease with increasing levels of income inequality. Taken together, the study’s findings suggest that racial segregation is bad for Blacks and explains the higher mortality rates associated with income inequality among Blacks.
Neighborhood residents may find it easy to observe how residential segregation unequally distributes trees or the frequency of violence, but they might not be able to see how residential segregation is "getting under the skin." In a study published in 2011, Mahasin Mujahid, with Kiarri Kershaw, Ana Diez Roux, Sarah Burgard, Lynda Lisbeth, and Amy Schultz, found evidence of a strong correlation between residential segregation and hypertension disparities.
The research team sought to identify environments where the Black-white hypertension disparities were smallest or nonexistent in order to learn if context perpetuated Black residents’ unequal burden of hypertension. They used a national set of health data to identify people with hypertension and assessed residential segregation at the census tract level. The analysis found that Black people living in low segregation areas were 1.67 times more likely to have hypertension than whites, and Black people living in high segregation areas were 3.57 times more likely than whites to have hypertension.45
This startling difference is evidence of a connection between neighborhood context and a specific measure of health. While a biological mechanism for the relationship between hypertension and place is still unknown, the findings offer valuable insights. It is hypothesized that residential segregation leads to health disparities because it concentrates Black people into high poverty areas, and living in poverty is associated with many neighborhood characteristics that are bad for health. This includes decreased neighborhood safety, limited access to healthy foods and recreational resources, and lower levels of educational attainment. However, Mujahid’s results suggest that neighborhood poverty alone cannot account for the stark Black and white hypertension differences.
In Figure 10, we see how the researchers consider segregation, neighborhood poverty, and race differences in hypertension together. Living in a low segregated area is associated with lower predictability of hypertension for Black people across low to high poverty neighborhoods than living in a high segregated area. The data also illustrate how Black and white differences in hypertension diminish as neighborhood poverty increases because predicted probability of hypertension in whites increases as neighborhood poverty increases. Therefore, when the three factors—segregation, neighborhood poverty, and differences in hypertension—are considered together, race differences in hypertension were greatest in segregated, low-poverty areas.
As the Haas Institute Diversity and Health Disparities research cluster members’ research findings show, residential segregation shapes racial disparities in health outcomes, neighborhood social conditions, and environmental features. As one scholar argues, “racial residential segregation and social inequality are fundamental causes of racial/ ethnic disparities in neighborhood physical and social environments.”46 This research suggests that addressing and reducing residential segregation benefits the public’s health and may reduce racial health disparities.
Conclusion
RACIAL AND ETHNIC health disparities are a persistent concern in the United States. These differences endure across gender, income, education, and at every point along the life course, despite national coordinated strategies to reduce them.
A growing body of innovative research from the Diversity and Health Disparities research cluster at UC Berkeley's Haas Institute for a Fair and Inclusive Society shows evidence for the missing link in our understanding of racial health disparities: neighborhood conditions. Their findings are consistent with the idea that inequality of neighborhood conditions shapes inequality in health outcomes.
Fewer trees and more asphalt creates hotter neighborhoods that endanger the health of residents who are vulnerable to extreme heat. Communities that are majority people of color and low income are exposed to greater concentrations and more kinds of harmful chemicals through the air in their neighborhoods due to their proximity to local sources of pollution. Black and white disparities in hypertension and cardiovascular disease can be explained by discrepancies in neighborhood conditions and residential segregation. Investigating the impact of neighborhood differences helps us see how health is shaped by the social and physical environment, not just medical care.
Policymakers must pay attention to the effects of all policies—not just health policies—on population health outcomes. As research shows, decisions that affect neighborhood safety, air quality, tree cover, and housing affect health, too. Similarly, policies that ignore health may unintentionally cause harm to communities that are over-burdened by preventable chronic diseases. While it may seem daunting for some government agencies to consider the health impacts of their work for the first time, evidence from municipal and state governments around the country shows that it is possible and that the outcomes are worth the effort.
- 1Jones, 2000
- 2Pastor & Morello-Frosch, 2014
- 3CMS, 2017
- 5Diez Roux et al., 2016
- 6Diez Roux et al., 2016
- A a b c d Krieger et al., 1997
- BChetty, et al., 2014
- CRichardson & Nuru-Jeter, 2012
- 7Kramer et al., 2004; Mensah et al., 2005; Weinsier et al., 1998
- 8http://www.cvriskcalculator.com/
- 9American Heart Association, 2018
- 10Cutler, 2004; Frohlich & Potvin, 2008
- 11Obasogie, et al., 2017; Keppel, 2007; National Center for Health Statistics, 2012
- 12 a b Nuru-Jeter et al., 2018
- 13 a b Nuru-Jeter et al., 2018
- 1.1Safford et al., 2012
- 2.1Carnethon et al., 2017
- 3.1Nuru-Jeter et al., 2009; Carnethon et al., 2017
- 4.1Baker et al., 2006
- 5.1Yancey, 2009
- 6.1Dias, 2013
- 7.1Zhang et al., 2017
- 8.1Powell-Wiley et al., 2017
- 9.1Tamayo et al., 2016
- 10.1Mujahid et al., 2017
- 11.1Carnethon et al., 2017
- 14Corburn et al., 2006
- 15Johnson, 2012
- 16Geronimus, 2006
- 17Johnson, 2011
- 18Herd et al., 2015
- 19Vinikoor et al., 2008; Pickett et al., 2005
- 20Cummins, 2007
- 21Wallerstein et al., 2018
- 22Participatory Budget Project, https://www.participatorybudgeting.org
- 23Youth-led Participatory Action Research, http://yparhub.berkeley.edu/
- 24Peoples Movement Assembly, http://www.peoplesmovementassembly.org/
- 25Place Matters team at the Alameda County Public Health Department, http://www.acphd.org/social-and-health-equity/policy-change/place-matte…
- 26Brody et al., 2009
- 27Brody et al., 2009
- 28Basner et al., 2014
- 29Casey et al., 2017
- 30Casey et al., 2017
- 31NRDC, 2017
- 32Jesdale et al., 2013
- 33Jesdale et al., 2013
- 34Borden & Cutter, 2008
- 35Meehl & Telbaldi, 2004
- 36Heynen et al. 2006; Landry & Chakraborty 2009; Lowry et al. 2012; Ogneva-Himmelberger et al. 2009; Perkins & Heynen 2004; Zhang et al. 2008
- 37Williams & Collins, 1995; Bailey et al., 2017; Braveman, 2017
- 38Berezin et al., 2017
- 39Berezin et al., 2017
- 40Wilson, 1987
- 41Nuru-Jeter et al., 2014; Backlund, E., et al., 2007; Kaplan, G. A., et al., 1996
- 42Lynch & Kaplan, 1997; Cooper et al., 2001; Deaton & Lubotsky, 2003
- 43Massey & Denton, 1993; Nuru-Jeter et al., 2014
- 44Nuru-Jeter et al., 2014
- 45Kershaw et al., 2011
- 46Casey et al., 2017